
New York suffered badly during spring 2020, but an unnamed doctor said 'looking back, we definitely could have prevented so many deaths by not putting people on ventilators'
Credit: BRYAN R. SMITH/AFP via Getty Images
Coronavirus Article Bar with counter
The patient lay prone on the emergency room bed. His oxygen levels – registering far below a healthy 95 per cent – were cause for concern but he was still able to breathe on his own.
“Is this one for ICU?” the attending doctor asked his supervisor as he pulled open the paper-thin blue hospital curtain.
“No, just monitor him on 100 per cent oxygen for now,” replied the head of the ER, a pulmonology specialist at a community hospital in New York, who has treated hundreds of Covid-19 patients since the outbreak crippled the city in March.
“We had been trained to intubate, intubate, intubate when a patient gets into difficulty,” said the ER chief, who manages a floor of 25 beds. “That’s what we were doing until we figured out it was killing people. Looking back, we definitely could have prevented so many deaths by not putting people on ventilators.”
The Telegraph returned to the emergency room of a hospital in New York City it visited during the height of the first wave of the pandemic in mid-April.
The doctor allowed us rare access to show the reality of what frontline workers have been facing, but on condition that neither he nor the hospital were named.
As New York experiences another surge, the doctor said the hospital was once again close to capacity. However, this time around he was not so fearful.
“The disease has changed,” the doctor told The Telegraph. “It’s much less dramatic than what we were seeing, far fewer are dying,” he said.
“I used to walk into the ER past the freezer truck morgues parked outside the entrance and for the first time in my career I was scared. Every day we were seeing death. Now we’re in the heart of the second phase, but we’re much more confident.”
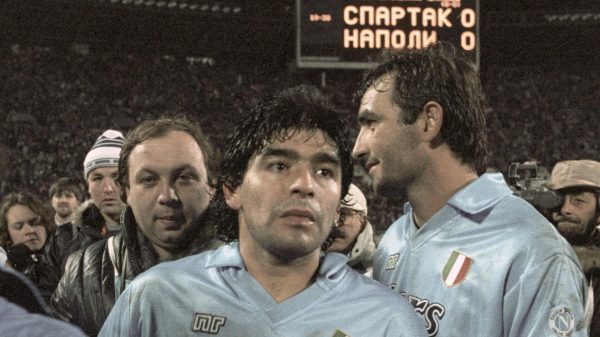
The countries with the highest Covid infection rate
Back in April, the ward was unnervingly quiet. Every bed was taken up by patients who lay unconscious as intubation tubes did their work. There was a palpable sense of panic among the physicians, who could not figure out what they were doing wrong.
During the last visit, the prone patient in the corner (a man in his mid-40s) let out a stirring cough before taking a sharp intake of breath. The ward was now a cacophony of sound, a comforting sign of life.
The man has been in for five days now and his condition has neither improved, nor deteriorated to the point of needing a ventilator.
“We have learned not to overreact when oxygen levels drop,” the doctor explained. “We were too keen to put people on ventilators when that should have been the last resort.”
According to research published in medical journal Clinical Infectious Diseases, ICU patients receiving mechanical ventilation had a 70 per cent mortality rate, compared to 21 per cent of hospitalised patients not requiring intubation.
Managing a patient on a ventilator is a time-consuming, delicate task that requires caregivers to monitor and adjust the amount of oxygen they are receiving, the pressure in their lungs and the time between breaths, among other factors, the study noted.
When hospitals in New York, China, and Italy were swamped with patients early in the pandemic, that simply was not possible.
The ventilator tubes also inflame tissue, which can interfere with breathing, and make it much more difficult for a patient to recover if they are taken off.
Doctors now believe intubation should only be done in extreme cases and, where possible, a patient should be given a less intrusive course of 100 per cent oxygen.
Patients in the UK on ventilators, in a video taken at the end of last April:
The doctor, who himself contracted the virus shortly after our visit, said the number of patients the hospital was placing on ventilators had fallen from two or three a day to two or three a week.
Some 30-35 per cent of the hospital’s 110 ER and ICU patients are in with Covid-19. Back in April, the percentage hovered around 98 per cent.
The doctor said fewer than five per cent of Covid-19 patients he has treated over the last month have died, a decline from nearly 30 per cent in Spring.
In April and May, the state’s daily death tolls were regularly exceeding 700. On Thursday, it recorded 144 deaths.
“Whatever is going around New York now has less efficacy, it’s like we’re seeing a much weaker strain of the virus,” the doctor said, who cautioned that he could not speak for other parts of the country. California, by comparison, recorded 442 deaths on Thursday, having been spared the worst of it in Spring.
The doctor compared what the UK was seeing now with what New York saw during the first wave. “It’s like they are experiencing what we did in reverse,” he said. "The non-stop wailing of ambulance sirens, the lines outside hospitals. We were there, but, for now at least, we’re not now."
Map of coronavirus cases and deaths worldwide
New York got its spring surge under control by implementing widespread testing, contact tracing, as well as phased lockdowns. Leaders also developed consistent messaging about necessary precautions.
Where New York City, which has a similar population size and density to London, set the terms of its own lockdown, the UK capital’s response depended mostly on guidelines set for the entire country.
The doctor also noted a drop in the average age of patients in his ER, which may be because a sizable percentage of the city’s over-65s contracted the virus in the first wave and those who did not have mostly been sheltering in place.
The doctor says his hospital in Brooklyn has seen a spike in hospitalisations since the Thanksgiving and Jewish Rosh Hashanah holidays in November.
Earlier this month they admitted a father with his 43-year-old son and a 87-year-old woman with her 94-year-old husband, all of whom had spent Thanksgiving with their families despite advice from the Centers for Disease Control and Prevention not to mix households.
“We treated them with a cocktail of Remdesiriv, blood thinners and oxygen, and the elderly couple were sent home,” said the doctor, who used to dread receiving older patients as they were more likely to end up on ventilators. “The mortality rate was shocking for a time,” he says.
Almost 8,000 Covid-19 patients are now hospitalised across New York State, double the amount reported in just a month ago, and the highest total since May 22, when 19,000 were admitted.
Andrew Cuomo, New York Governor, said the state is not yet at a “critical level”, but warned he was prepared to reactivate the 2,500-bed makeshift hospital at the Javits Center if numbers rise any higher.
The biggest problem hospitals in New York now face, the doctor warned, is staffing. Private hospitals like his have been forced to lay off higher-paid doctors as they struggle to plug the funding gap left by the huge drop in elective surgeries.
Others either quit or retired early amid low morale, reflecting a growing trend across the state. Some 1,000 workers walked off their jobs at health centres in upstate cities of New Rochelle and Albany, complaining of being overworked and given inadequate protection.
Mr Cuomo has said potential staff shortages is now a greater concern than available beds for patients. He has even asked hospital officials in the state to identify retired doctors and nurses to help over winter.
At the Brooklyn hospital, the ER chief said he has taken to starting his shift at 3am and finishing at 9pm as there is no one to hand over to until late in the evening.
“I’m worried what will happen in the new year if we lose any more doctors,” he said. “It’s no good having the treatment if we don’t have the staff to administer it.”



















































Свежие комментарии