This is not the first time that a pandemic has gripped the holiday season. In December 1918, preparations for the first Christmas without war in four years took place in the midst of the worst pandemic since the Black Death.
The 1918-19 influenza, like Covid-19, came in waves. The deadliest began in autumn, peaked in late November and continued through the first weeks of December. It struck hundreds of millions and killed tens of millions worldwide.
One quarter of Britons were ill with the virus and 225,000 died, most in the months and weeks before Christmas.
But while there are similarities between the two pandemics – both are highly infectious respiratory diseases that spread in waves – there are also important differences in the contexts in which they developed, in efforts to control them, in their impact on healthcare systems and how people learned to live with them.
People celebrating Christmas and other seasonal holidays in 1918 faced nothing like the restrictions people will face this year.
The reasons for this difference are many, looking at a few can offer some lessons.
The experience of the 1918 pandemic was intimately tied to the first world war, which not only facilitated its rapid spread but also significantly shaped the responses to it.
Until the armistice in November 1918, winning the war had been more important than the battle against influenza.
In Britain, public health, military and government officials counselled the nation to “carry on” in the face of the escalating and worsening pandemic.
Britain’s chief medical officer of health, Sir Arthur Newsholme, issued the first official memorandum in October. It recommended a range of measures to slow influenza, including isolating the sick from the healthy, school and cinema closures, oral disinfection (gargling with antiseptics), and warnings against large “aggregations of people”.
Mask-wearing was not among the recommendations.
None of the measures was mandatory and responsibility for their implementation fell to local authorities, who adopted them in a piecemeal manner.
Medical officers and local authorities in London took diverging approaches, with some closing cinemas and schools, while others hardly intervened. By contrast, in Manchester, the medical officer of health, Dr James Niven, developed a vigorous scheme of prevention and treatment, which likely mitigated the epidemic: whereas the second wave peaked in London in the second and third week of November, it peaked in Manchester in early December.
There are a number of reasons why measures were not systematically introduced. War demands were important. Medical experts were uncertain about the identity of the epidemic: who it most affected, the nature and severity of symptoms, and how it killed did not conform to what was known about influenza.
Most authorities thought that influenza was caused by a bacillus, but systematic testing was impossible because it was difficult to isolate from the sick and to grow in cultures.
Public attitudes mattered. Influenza was widely viewed as little more than a burdensome but mostly mild malady. People who had already endured four years of wartime privations were unlikely to welcome or comply with severe restrictions.
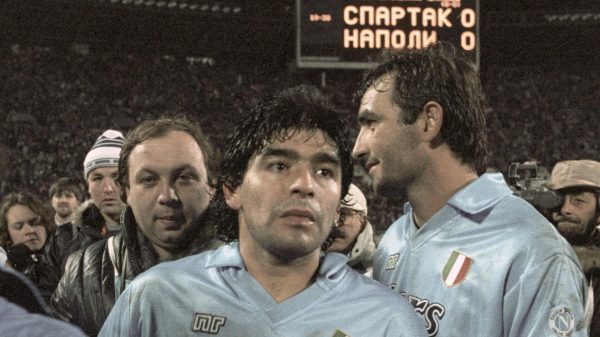
This was especially the case when the war ended. It is no coincidence that the second wave peaked after armistice, when thousands defied public health advice and massed together to celebrate in squares, streets, pubs, homes and churches across the country.
Soon thereafter, decommissioned soldiers brought influenza back to Britain or carried it home to India, Australia, New Zealand, Canada, the US and beyond.
As the epidemic continued through November and early December, hospitals were overwhelmed by the influx of the sick and dying. Most were understaffed because at least half of Britain’s nurses and doctors had been commissioned for the war effort.
Those on hand could offer little more than nursing or palliative care: there were no effective treatments against influenza or the deadly pneumonic complications that accompanied the disease. While the sick were encouraged to seek medical attention, most suffered and died in their homes, under the care not of a doctor or nurse, but of a family member, friend or neighbour.
Burials were halted in places because of shortages of caskets. By early December, a growing number of schools were closed, either as a precaution or because teachers and students had fallen ill. Just as now, schoolchildren were thought to be spreaders of infection, and school closures were viewed as a necessary but controversial measure.
William Hamer, the chief medical officer of the London county council, opposed school closures on the grounds that “such action would simply release the children and allow them to congregate in places where danger of infection is greater”.
In early December, Manchester decided to close all elementary schools until the new year. Such measures were a double-edged sword.
Unlike today, children were not locked down in their homes. The majority simply ended up playing together on local streets or parks and, just as Hamer feared, further spreading the disease.
By Christmas Day, the second wave had largely subsided. The lull offered time for reflection and gave rise to expressions of loss, anger and hope. Shadowed by the twin tragedies of the war and the pandemic, this was a Christmas like no other.
Obituary pages of national and local newspapers, which had been filled with war deaths, were now also filled with influenza deaths. Stories abounded of young men who had survived the western front only to perish from influenza on their return.
The Times reminded readers that “this plague … generally regarded with equanimity, is, it would seem, five times more deadly than the war.” It estimated that “some 6 million persons have perished of influenza and pneumonia during the past 12 weeks.”
The number was a massive underestimate. Weeks later, the paper would revise the global figure upwards to 12 million, but even this figure was too low.
Along with a collective sense of loss, the season also unleashed anger. Most of it was directed at the failure of public health authorities to prevent the pandemic.
The Manchester Guardian’s medical correspondent decried that the epidemic “has revealed the relative helplessness of preventive medicine in the face of certain infections.”
Newsholme and his department were especially targeted for their failure to coordinate an effective national response. There were calls for Lloyd George’s newly elected government to accelerate the creation of a ministry of health to put the nation’s preventive system on a better footing.
The sharpest criticisms turned on the failure to recommend the general use of gauze masks to prevent the spread of infection. Critics questioned why mask-wearing on trains, omnibuses and public places had not been made a general measure. They pointed to the example of San Francisco, where a city-wide mask order had reportedly stamped out the epidemic.
Mask-wearing became part of a public discussion about the medical and cultural changes needed to prepare for future epidemics. The Manchester Guardian wondered whether this measure said something about the British character: “It is possible that only our British self-consciousness has prevented us from taking the precaution of wearing germ masks during influenza epidemics.”
As the second wave abated, there was some optimism that the worst was over. There was hope that a new influenza vaccine, which had been developed by the War Office and tested on military populations, would become widely available to the public.
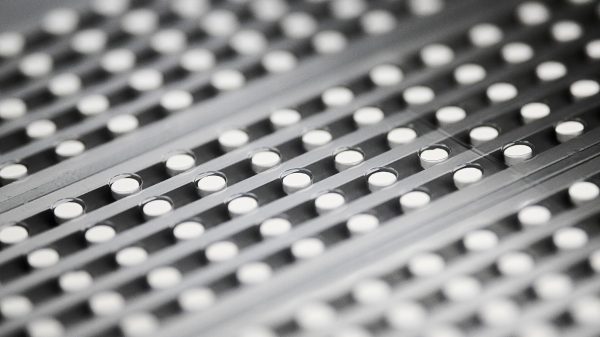
Made from a mixture of bacteria, the vaccine proved to be moderately effective against secondary infections like pneumonia, but did not protect against influenza. Nonetheless, demand was high and manufacturers rushed to supply local authorities.
Influenza returned shortly after the new year. Although less widespread and severe, the third wave was likely seeded during the Christmas period. It was a stark reminder that this epidemic disease would remain a regular visitor.
Ultimately, Britons and people around the world had to learn to live with influenza. Just as with Covid-19, this meant dealing with grievous loss, acknowledging systematic failures, and developing new ways of managing epidemics.
The virus that caused such devastation in autumn 1918 circulated for decades in a milder form but still caused outbreaks and epidemics. Influenza deaths and illness became an accepted part of modern life, figuring into the rational calculus of health care and insurance systems, and the experiences of individuals, families and communities.
Every pandemic is a step into the unknown. We need to bear in mind differences in the worlds in which influenza and Covid-19 emerged, in the state of medical and scientific knowhow, in health care infrastructures, and in capacities to respond.
Looking backwards should remind us that each pandemic brings with it unique problems that require unique solutions.
Britain and the world in 2020 are in a far better position to tackle a pandemic then ever before. But as 1918 shows, even with best available medicine and science, communities and nations have to learn to live with epidemic diseases. The challenge is to learn to live well with them; this is something few people were able to do in 1918.
Michael Bresalier, Department of History, Swansea University. His forthcoming book is called, The Viral Pandemic: Science, medicine and the making of modern influenza.























































Свежие комментарии